The demand for palliative care in Sri Lanka continues to grow due to the rising prevalence of non-communicable diseases and the ageing of the population. Palliative care is well recognised and resourced as an integral component of the health system in Sri Lanka’s national policy. It is included in the National Strategic Framework for Palliative Care Development in Sri Lanka (2019-2023) and the National Strategic Plan in Prevention and Control of Cancer in Sri Lanka (2020-2024). The writer argues once more for the Provincial health services to burden share in this vital healthcare need.
We have an aging population as well higher reported incidents of non- communicable diseases. Caring and costs associated have proven challenging. The Dean Faculty of Medicine, UoJ and the Deputy Director, JTH have championed organised community based palliative care services in the Northern Province, replicable across SL. The Kerala experience is very encouraging and culturally adaptable in SL.
Palliative care is specialised medical care for people living with a serious illness. This type of care is focused on providing relief from the symptoms and stress of the illness. The goal is to improve quality of life for both the patient and the family.
 Palliative care has evolved from an almost exclusive focus on end-of-life, late-stage patients in inpatient settings to a more interdisciplinary specialty that addresses the needs of seriously ill persons in their homes. Palliative care services include symptom management, customised plans of care, social services, and advance care planning.
Palliative care has evolved from an almost exclusive focus on end-of-life, late-stage patients in inpatient settings to a more interdisciplinary specialty that addresses the needs of seriously ill persons in their homes. Palliative care services include symptom management, customised plans of care, social services, and advance care planning.
Who needs palliative care?
People with various conditions receive palliative care. Among many others, these conditions include: Amyotrophic lateral sclerosis (ALS), Alzheimer’s disease, Cancer,COVID-19, Chronic obstructive pulmonary disease (COPD), Heart disease, HIV & AIDS, Kidney disease, Liver disease, Lung disease, Multiple sclerosis (MS), Parkinson’s disease, Stroke and some types of psychological afflictions.
Palliative care teams include medical providers and other specialists who can help you manage symptoms. They can also help you navigate the added stress and responsibilities that often accompany serious illnesses.Your care team may include:Doctors,Nurses,Social workers,Nutritionists, Financial advisors, Spiritual advisors.
Depending on the resources available in your area, you can receive palliative care in a variety of locations, including:Home, Assisted living facility,in a nursing home,Outpatient clinic and Hospital.
Palliative care can help improve symptoms affecting your physical, mental and emotional well-being. Your palliative care team may deliver care directly. They may also teach you strategies you can use every day to feel better.
Palliative care can help with: Anxiety, Depression, Nausea, Fatigue, Constipation, Pain or discomfort, Trouble sleeping, Lack of appetite, Shortness or Stress.
Your palliative care team may provide: Tips for improving sleep, Cognitive exercises, Relaxation exercises, Breathing exercises, Nutrition guidance, Exercise guidance, Talktherapy, Healing touch, Meditation and Massage. Palliative care providers can also refer you to specialists if you need additional care.
Kerala model of palliative care
Kerala, in India, has shown enormous progress in the area of palliative care (PC). Most of it is due to the network of community initiatives in PC in north Kerala. This network, called “Neighbourhood Network in Palliative Care,” has more than 60 units covering a population of more than 12 million, and is probably the largest community-owned PC network in the world. The Kerala Model places a strong emphasis on community participation and volunteerism integrated with Primary Healthcare system especially through dedicated nurses under the overall leadership of local governments.
Under the program, people who can spare at least two hours per week to care for the sick in their area are enrolled in a structured training program (16 hours of interactive theory sessions plus four clinical days under supervision). On successful completion of this “entry point” training (which includes an evaluation at the end), the volunteers are encouraged to form groups of 10–15 community volunteers and to identify the problems of the chronically ill people in their area and to organise appropriate interventions. These NNPC groups are supported by trained doctors and nurses.
NNPC groups usually work closely with the existing PC facilities in their area or build such facilities on their own. Volunteers from these groups make regular home visits to follow up on the patients seen by the PC team. They identify and address a variety of nonmedical issues, including financial problems, patients in need of care, organising programs to create awareness in the community, and raising funds for PC activities. Community volunteers act as the link between the patient in the community and the healthcare provider in the institution.
NNPC does not aim to replace health care professionals with volunteers. Instead, what is being attempted is to supplement the efforts of trained doctors and nurses in psychosocial and spiritual support by trained volunteers in the community. Groups of trained volunteers are tied to PC professionals and health care facilities in their communities. The action plans clearly define individuals’ and institutions’ roles and responsibilities. In between the reporting to the outpatient clinic/inpatient unit by the patient/family, the local volunteers visit the patient at home. Such visits supplement the visits by the home care team. Such visits result in better emotional support, better compliance with medical/nursing instructions, earlier reporting of symptoms to the doctor, and social, including financial, support. In addition, in places where NNPC is active, patients in need are identified early. The program is characterised by-
- A focus on care at home with outpatient clinics and inpatient units acting in support
- Attention to social and emotional well-being as much as physical health
- Mobilisation of resources locally
- The building up of skills and confidence in the local community
A network with more than 4,000 volunteers, and 36 doctors and 60 nurses looking after about 5,000 patients at any point of time. All the doctors and nurses in the network are those employed by the community initiatives.
Community Based Palliative Care Model
Within less than five years, the NNPC initiatives have resulted in the establishment of 68 community-based PC initiatives in northern and mid-Kerala, covering a population of more than 12 millione.g., PC for patients with non-malignant conditions, including chronic psychiatric disorders; and active involvement of the local government in providing care for the chronically ill and incurable patients in the region.
Most of the PC services are either doctor or nurse led. But when we look at the needs and problems of those with long-term and incurable illnesses, we find that they are also of a psychosocial and spiritual nature. Social needs assume importance, especially in the developing world. Medical professionals have only a minor role in this scenario and that is to help in alleviating the symptoms. Issues related to incurable and chronic illnesses are essentially psychosocial and spiritual problems, with a strong medical/nursing component. The solutions for these problems need to be explored in the community itself.
Community is not monolithic. It is heterogeneous, with wide differences in socioeconomic status, educational status, religion, ethnicity, and so on. The extent of participation of people from the poor and middle class strata of the society has been one of the main characteristics of the NNPC program.
What is being observed in the PC scene in northern Kerala can probably be described as a “palliative care version” of a community initiative. The NNPC experiment has also shown that it is possible to bring individuals and groups with different social, religious, and political perspectives together on a broad spectrum of social justice issues to work for marginalised people in the community.
This particular social experiment has the potential to offer a good number of lessons in many areas of healthcare and development today. Development of PC services in most regions of the world, issues related to community participation in health care, and community participation (or lack of it) in development projects are some of them.
***************************
Strategies recommended for provincial services
1. Ensure that palliative care is recognised and resourced as an integral component of the health system by making palliative care as an essential component of comprehensive health care.
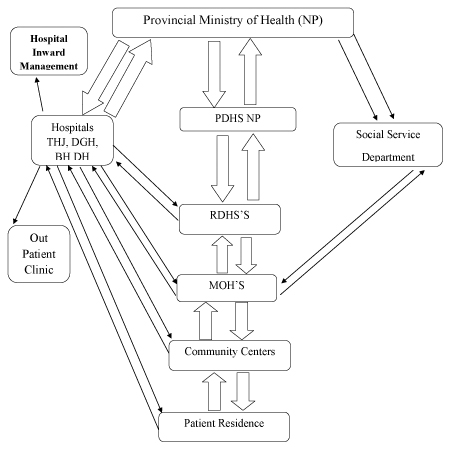
2. Facilitate the effective integration of specialist palliative care and palliative care services across all levels of service settings, namely at tertiary, secondary, primary and at community level.
3. Develop and make available skilled multi-disciplinary human resources and infrastructure for delivery of palliative care services at institutional and at community levels.
4. Ensure that patients and their families receive palliative care services they need when and where required & adherence to protocols & guidelines in palliative care.
5. Ensure availability of essential drugs & technologies for provision of palliative care at all levels: tertiary, secondary, primary and community level.
6. Build partnerships with government and non-governmental organisations for delivery of palliative care.
7. Empower family members, care givers and general public for the provision of palliative care.
8. Encourage research related to palliative care in assessing needs for palliative care and suitable models for implementation of palliative care services.
9. Ensure adequate financing & resource allocation for cost effective delivery of palliative care.
10. Strengthen legislative framework for delivery of palliative care.
11. Ensure monitoring & evaluation framework for palliative care services.
Jeevan Thiagarajah




